
IDENTIFICATION AND ASSESSMENT OF EVIDENCE

– Diagnosis and management of conjoined twins.– Management of monochorionic monoamniotic (MCMA) twin pregnancy.– Screening, diagnosis and management of TAPS.– Screening, diagnosis and management of TTTS.Complications unique to monochorionic twin pregnancy.Management of multiple pregnancy complicated by single IUD.Screening, diagnosis and management of FGR.Diagnosis and management of discordant twin pregnancy.Timing, frequency and content of ultrasound assessment.Determining chorionicity and amnionicity.Dating of the pregnancy (determining gestational age).The management of higher-order multiple pregnancy will be covered in a separate document. The document provides guidance on the methods used to determine gestational age and chorionicity, screening for chromosomal and structural abnormalities, and screening for TTTS, TAPS, growth abnormalities and preterm birth. This guidance will address the role of ultrasound in the care of uncomplicated twin pregnancy and those complicated by TTTS, selective FGR (sFGR), twin anemia–polycythemia sequence (TAPS), twin reversed arterial perfusion (TRAP) sequence, conjoined twins and single intrauterine death (IUD). As in singletons, impaired fetal growth can be assessed in twins by comparing biometry and Doppler velocimetry parameters against standards for uncomplicated pregnancy. Ultrasound assessment of fetal biometry, anatomy, Doppler velocimetry and amniotic fluid volume is used to identify and monitor twin pregnancies at risk of adverse outcomes such as twin-to-twin transfusion syndrome (TTTS) and fetal growth restriction (FGR). The risk is significantly higher in monochorionic compared with dichorionic pregnancy 3- 6. In addition, compared with singletons, twins are at increased risk of iatrogenic preterm delivery due to the greater incidence of maternal and fetal complications. Of course, such complications rise with a reduction in gestational age at birth.
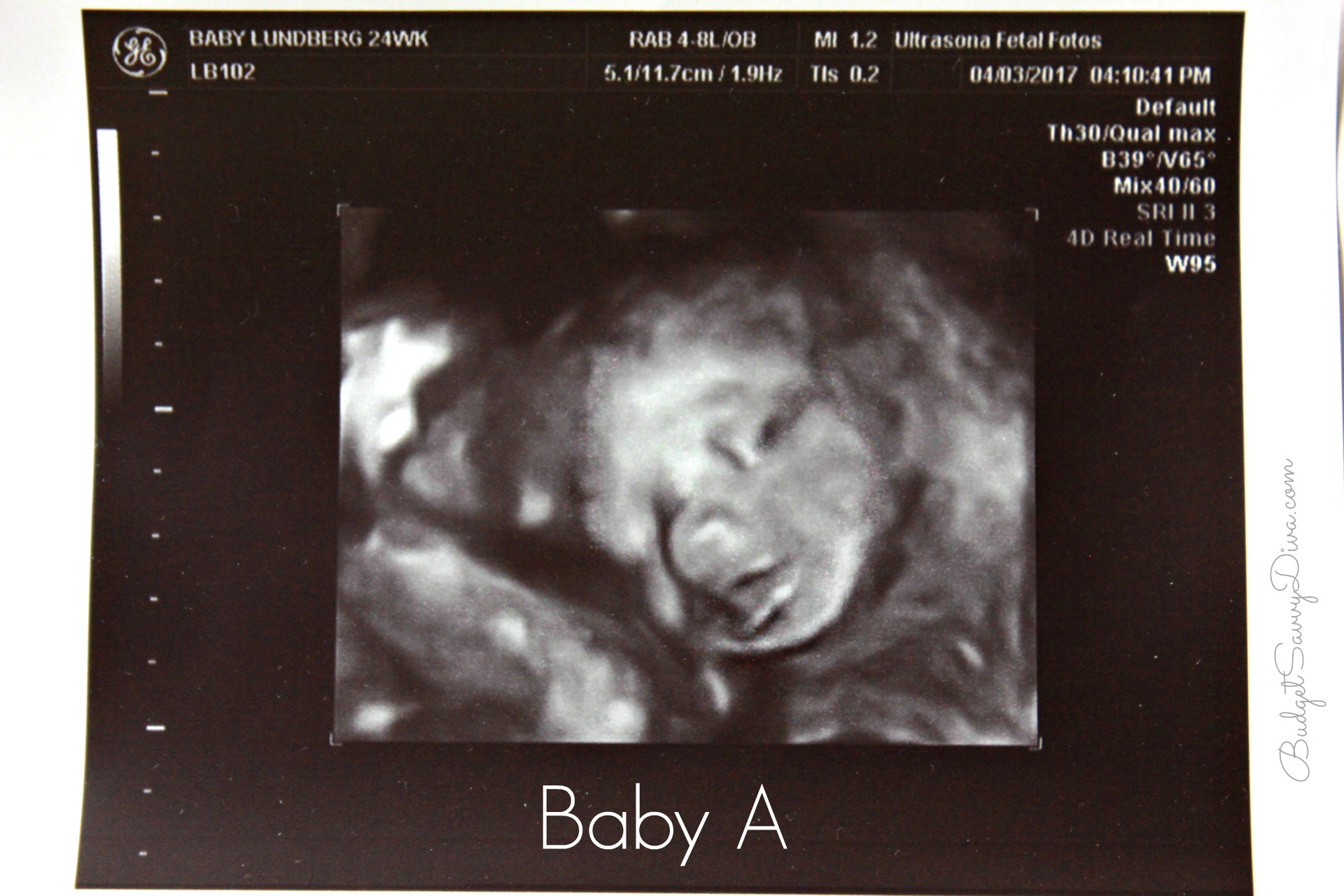
/twin-pregnancy-ultrasound-pic-56a68a3d5f9b58b7d0e3713c.jpg)
Preterm birth prior to 37 weeks' gestation occurs in up to 60% of multiple pregnancies, contributing to the increased risk of neonatal mortality (65% of neonatal deaths among multiple births are preterm, compared with 43% of neonatal deaths in singletons) and long-term morbidity 9- 12. In 2009, the associated stillbirth rate was twin births and triplet and higher-order multiple births, compared with five per 1000 singleton births 7, 8. Twin pregnancy is associated with a high risk of perinatal mortality and morbidity 3- 6. The twin birth rate increased by just under 70% between 1980 ( live births) and 2006 ( live births) 2. The incidence of multiple pregnancy is rising, mainly due to delayed childbirth and advanced maternal age at conception and the resultant widespread use of assisted reproduction techniques 1. Approved Guidelines can be distributed freely with the permission of ISUOG ( INTRODUCTION
The ISUOG CSC documents are not intended to establish a legal standard of care because interpretation of the evidence that underpins the Guidelines may be influenced by individual circumstances, local protocol and available resources. Although ISUOG has made every effort to ensure that Guidelines are accurate when issued, neither the Society nor any of its employees or members accepts any liability for the consequences of any inaccurate or misleading data, opinions or statements issued by the CSC. They are intended to reflect what is considered by ISUOG to be the best practice at the time at which they are issued.

The ISUOG Clinical Standards Committee (CSC) has a remit to develop Practice Guidelines and Consensus Statements as educational recommendations that provide healthcare practitioners with a consensus-based approach, from experts, for diagnostic imaging. The International Society of Ultrasound in ObstetricsĪnd Gynecology (ISUOG) is a scientific organization that encourages sound clinical practice, and high-quality teaching and research related to diagnostic imaging in women's healthcare.


 0 kommentar(er)
0 kommentar(er)
